Interview with a Soapbox Scientist: Dr. Katie Partridge
Most of us know somebody with diabetes. It’s a disease that is becoming more prevalent in the UK, which is concerning not only for those directly and indirectly affected by it, but also for our struggling healthcare systems. The organ that malfunctions in diabetes is the pancreas. In healthy people, the pancreas regulates blood sugar so that if levels get too high or too low, it releases hormones to bring those levels back into a healthy range. In people with diabetes, the organ doesn’t function as it should, and blood sugar levels can get dangerously out of control. But how exactly does a pancreas carefully orchestrate the balancing act of keeping our blood sugars in the right range?
While it’s easy to think of organs as lumps of tissue, there are entire, intricate worlds inside of them that are constantly working to keep our bodies functioning as they should. Dr. Katie Partridge, a postdoctoral researcher at the University of Exeter, tells me that the pancreas actually has a very complicated structure at the microscopic level. “The pancreas has several cell types that release hormones and work to regulate blood sugar levels. These cells are connected in little islands, called islets, inside the pancreas. The most common cell types in these islands are alpha and beta cells.” For anyone needing a refresher on what exactly a cell is, they are the building blocks of our bodies. Each part of our body has different, specialised cell types, such as red and white blood cells in our blood, and neurons in our brains. Alpha and beta cells are simply specialised, hormone-secreting pancreatic cells.
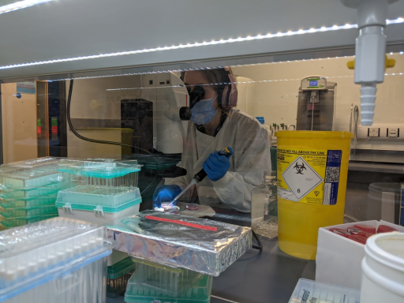
Katie working with pancreatic islets in the lab. Photo credit: Dr. Paul Weightman-Potter
Katie tells me that in a healthy pancreas, the alpha and beta cells within an islet are in constant communication with each other. “Beta cells release a hormone – insulin – to bring blood sugar levels down when it gets too high, especially after a meal. On the other hand, alpha cells release the hormone glucagon to bring blood sugar levels up when it gets too low. Importantly, these cells co-ordinate their responses by communicating with each other using specialised chemicals.” I ask Katie how exactly these cells know what levels of sugars are in our blood. She tells me that, although there is a lot we still need to learn about this, the alpha cells essentially act as direct sugar sensors by changing the cells’ electrical state, and using this information to respond to our blood sugar levels. It’s a clever little world inside a pancreas.
In people with diabetes, beta cells – the cells which release insulin in response to high blood sugar levels – are attacked and killed by the body’s own immune system. This means they can no longer function, and blood sugar levels can therefore get dangerously high. However, Katie tells me that we don’t know as much about the role of alpha cells. “We know a lot about beta cells. They’re the most common cells in the islets and they are the ones that are destroyed in diabetes. But alpha cells are really important for us to understand too. They are the second most common cell in the islets, and they are super important for responding to low blood sugar levels. We really don’t know much about them, though.” Katie spent her PhD, based at the University of Exeter, looking into alpha cells. “They’re quite often overlooked. Maybe that’s what drew me to them!”
You may wonder how exactly someone goes about studying a cell that sits within an organ that sits inside a body. I certainly did, and Katie’s answer was not what I expected. “We basically study these cells using immortalised alpha cells that originally came from rodents. We grow these cells in petri dishes in the lab, and we feed them with specific food so that they don’t die. Then we can run experiments on them to find out how they work.”
Katie explains, though, that the cells need quite a lot of care to stay happy. “I like to think of them as a Tamagotchi. They need things to be just right to be happy. And it sounds strange, but the longer you work with these cells, the better you get at knowing when they are unhappy. They just start to behave in a certain way that isn’t quite normal.” I ask Katie what a ‘happy cell’ means for her research, and she tells me that happy cells are key to reliable results. “If cells are unhappy, they won’t respond to an experiment in the same way as happy cells. The results wouldn’t be very informative. We’d be seeing what stressed out cells do in a specific context, rather than what a cell would normally do in that context.”
If Katie’s alpha cells are happy and therefore ready for an experiment, she exposes them to various experimental conditions to try to get a better understanding of what the cells do and how they do it. “For example, we can expose them to certain medicines. If we know exactly how a medicine works at the molecular level, then how the alpha cells respond to the medicine gives us clues as to how they function. In addition to that, we may find that some medicines work well in helping the alpha cells do what they need to do, which means that the medicine could be useful in diabetes treatment. This means our work can not only build on our understanding of how alpha cells function, but can also be helpful for finding drugs that might help people with diabetes.”
Katie recently passed her PhD viva (the ‘final exam’ in a PhD, where the student defends their work to a group of experts), meaning she is a newly minted doctor. “It’s been rocky at times, especially with the pandemic, and none of my immediate family have been to university so being able to achieve this – and getting through all the hurdles to get here – has been huge.” Katie tells me that she loved her viva, largely because she loves speaking about her research to others. “I just love talking about this topic, with friends and family and to a broader audience.” She tells me that the research is of particular relevance for her family, because she has multiple family members with diabetes. “That has really motivated me to do this work. And as diabetes becomes more prevalent, it’s so important that we keep doing this research. Understanding how pancreatic cells work will help with drug development, and that will make life better for all those affected by diabetes.”

