Unravelling the mysteries of the pancreas to improve type 1 diabetes diagnosis
25 January 2021
4 mins to read
Type 1 diabetes occurs when the body’s immune system attacks and destroys the insulin-producing cells in the pancreas. This means they no longer regulate blood sugar levels effectively and a person needs multiple daily insulin injections to do this job.
Getting the right diagnosis is a major problem, particularly for adults. Previously, type 1 diabetes was thought to be mainly a disease of childhood. Exeter’s research busted this myth, demonstrating that in people diagnosed over the age of 30, around half of adults with type 1 are treated as type 2, as happened to former prime minister Teresa May.
"Misdiagnosis means you end up on ineffective treatment" explained Dr Richard Oram. "In extreme cases, patients are at risk of a dangerous and potentially deadly complication called ketoacidosis."
In older adults, misdiagnosis can occur in the other direction, with patients with type 2 diabetes misdiagnosed with type 1 diabetes and given unnecessary insulin treatment.
Harnessing c-peptide to measure insulin secretion
One reason for mistakes in the correct diagnosis of type 1 diabetes is that it’s hard to know how much insulin a person continues to make once they are on insulin treatment. Measuring a patient’s insulin directly does not work, as it will measure both the insulin they produce and the insulin they are taking for treatment.
The Exeter team addressed this by developing simple, inexpensive ways to measure insulin secretion, by measuring C-peptide. This is produced when the pancreas makes insulin, but it’s not present in insulin injections. This means C-Peptide levels mimic the amount of insulin the body is producing. The team developed a new urine test to measure C-peptide, and simplified blood tests, and demonstrated that these tests could be used to inform clinical care.
Professor Angus Jones explained: "That research has had a huge impact. These tests are now used right across the UK and the world. This has meant many patients have been able to change to a more effective treatment."
"That research has had a huge impact. These tests are now used right across the UK and the world. This has meant many patients have been able to change to a more effective treatment."
Dr Angus Jones
Associate Professor, NIHR Clinical Scientist,
Consultant Physician
Combining genetic and clinical information to diagnose type 1 diabetes
In a separate tool to aid diagnosis, the team combined routine information such as a patient’s weight, age, and blood test results in a calculator to help diagnose whether a person has type 1 or 2 diabetes. In difficult cases, doctors can also add the results of a new Exeter-developed type 1 diabetes genetic risk score, a measure of the extent to which someone if predisposed to type 1 diabetes, which improves accuracy even further.
Dr Oram said: "It can often be hard for doctors to know if an adult has type 1 or type 2 diabetes when they first present, as many people have features that could suggest both conditions, for example they could be young but have a high body weight, or old and thin. This calculator allows doctors to accurately combine different information, to help people with diabetes get the right diagnosis, and best treatment."
The Exeter genetic risk score, which costs just pounds, can also help identify which babies are more likely to go on to develop type 1 diabetes. By combining this score with other information, Exeter researchers have created calculators to accurately predict a child’s risk of developing type 1 diabetes in the future.
Dr Oram said: "Recent Immunotherapy trials have shown that if you can accurately predict who will go on to develop type 1 diabetes, you can delay the onset, and perhaps in the future prevent some from ever developing the condition. That would be a huge achievement."

A future of preventing type 1 diabetes
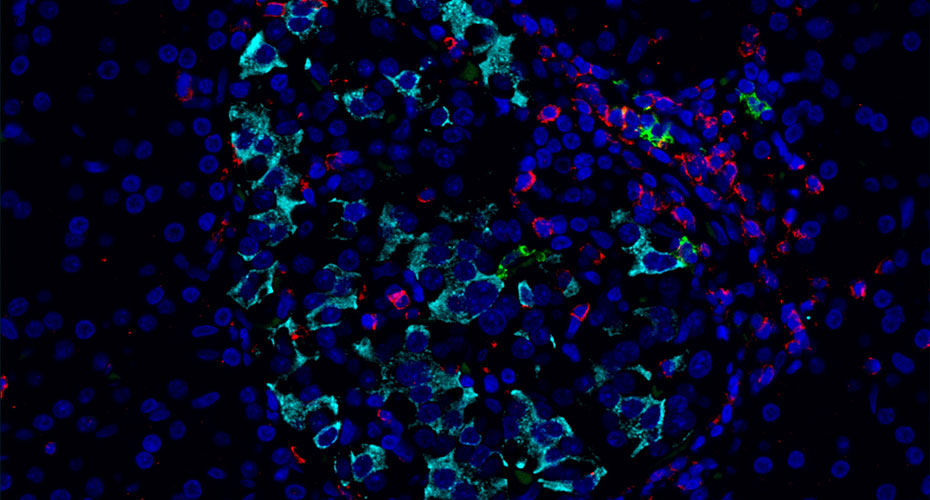
The pancreas has been hard to study in people, but now its secrets are being unlocked using a unique bank of samples from children who died shortly after being diagnosed with type 1 diabetes. "It’s very sad, but this is a unique resource in the world, and it’s incredibly precious in helping us understand the biology of type 1 diabetes," Professor Noel Morgan explained.
This biobank helped researchers analyse in detail how beta cells are attacked by the immune system. They were surprised to find distinct patterns which differed according to how old the child had been when they got type 1 diabetes. Combining this new knowledge with measurements of C-peptide developed in Exeter transformed our understanding.
"We began to see that what we thought was one illness, was actually really two. It differed in children under seven who had many more immune cells, and of a different type, compared to older teenagers. If we can understand which form of diabetes a child may get, we can target therapies to these particular cells in a precise way. We hope it will open the door to therapeutics that can stop people getting type 1 diabetes."
"If we can understand which form of diabetes a child may get, we can target therapies to these particular cells in a precise way. We hope it will open the door to therapeutics that can stop people getting type 1 diabetes."
Professor Noel Morgan
Professor of Endocrine Pharmacology
Explore more research
Precision diabetes: The right treatment for each patient
The University of Exeter has led the way in making discoveries that are swiftly translated into healthcare, to improve lives worldwide.

From gene discovery to revolutionising clinical care
When the Exeter diabetes lab was set up in 1995, medicine did not recognise that many forms of diabetes are caused by a single gene mutation.







